Dr. Shruti Mahajan, M12806, Dr. Rohit Om Parkash, Dr. Ajay Khanna, Dr. Trupti Mudholkar
PURPOSE OF THE STUDY:
To compare and evaluate the applicability of Keratograph corneal topographer for the diagnosis of dry eye with conventional methods.
INTRODUCTION:
It’s a well-known fact that the tear film is an important refractive surface.
The greatest change in refractive index occurs between air and the precorneal tear film, making the tear film critical to the optical power of the eye.
INFLUENCE OF TEAR FILM BREAK UPON QUALITY OF VISION:

In normal eyes, after a blink, there is a gradual increase in optical aberrations associated with the increasingly irregular tear film, which causes a progressive reduction in the optical quality of the eye (mean decrease 21%).All this is exaggerated in dry eye syndrome.
Clinically we can evaluate dry eye disease by slit lamp evaluation, various staining techniques and Schirmer’s test.

However, these are poorly associated / do not correlate well with the subjective symptoms.
Keratograph and its functions:
METHODS:
Study design :
A prospective, comparative study
30 patients
Subjected to :
- Clinical evaluation
- Keratograph (non contact) evaluation
(I) Clinical evaluation :
Signs and symptoms
- Tear Break up Time (TBUT)- fluorescein based
- Schirmer’s Test I
- Tear Film Meniscus height (TFMH) on slit lamp
- Slit lamp grading of Meibomian glands
(II) Keratograph Evaluation (Oculus Keratograph K5)
- Noninvasive break-up time of the tear film (NIKBUT)
- Tear Meniscus Height (TMH)
- Lipid layer interferometry
- Meibomian gland imaging
RESULTS:
There was moderate correlation between traditional and topographer tear film break up time values.
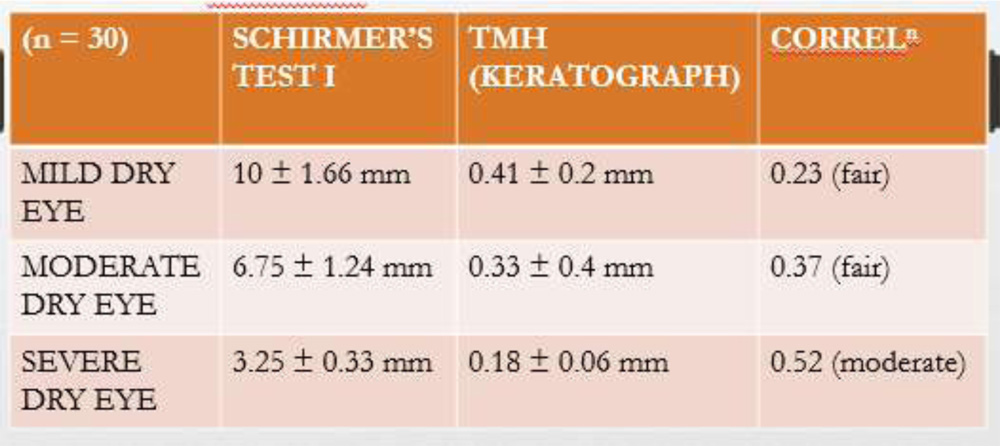
- Mean Schirmer’s test and TMH
- Inter-examiner reliability for the three clinical characteristics (telangiectasias, turbidity of meibum and gland dropout) were studied.
- Meibomian gland architecture evaluation showed less inter-observer variation with keratograph as compared to clinical evaluation.
EVALUATING AGREEMENT BETWEEN THE CLINICAL AND KERATOGRAPH IMAGE EXAMINER (Unweighted and Weighted к Values):

CONCLUSION:
An automated keratograph can provide a simple, and reliable non-invasive screening test for evaluation of structural and functional changes in dry eye with fair to moderate correlation with the conventional diagnostic tests.
WHAT IS KNOWN:
- There is no gold standard evaluation test for dry eye syndrome.
- Clinical evaluation can be subjective with moderate to high inter-observer variability.
WHAT THIS PAPER ADDS:
- Keratograph can provide more quantifiable, reproducible and accurate evaluation.
It correlates well with the clinical signs and symptoms and evaluation

